It’s not as simple as saying, “I will stop using today.” Once a person stops using an opioid after prolonged use, the brain goes into overdrive. Getting the brain back to its natural state, (whatever that means for you), could take a combination of medical and psychological therapies. Everyone is different and there is no “best” way of getting clean and sober. We just get there however it makes sense to us. The act of stopping is the first step toward recovery, after the realization and acceptance stage that is. Combining counseling, therapy, and the right people in your corner are all important factors. Providing those who take Suboxone all of these things are vital for long-term recovery. Suboxone works or “kicks in” within minutes for most patients. The very first dose must be taken while the patient is experiencing withdrawal symptoms. If Suboxone is taken too soon after the last ingested drug use, a risk of increased withdrawal symptoms can occur. While this “waiting” period can be quite uncomfortable, once Suboxone is administered, the patient is moments from relief.
Suboxone as an Option
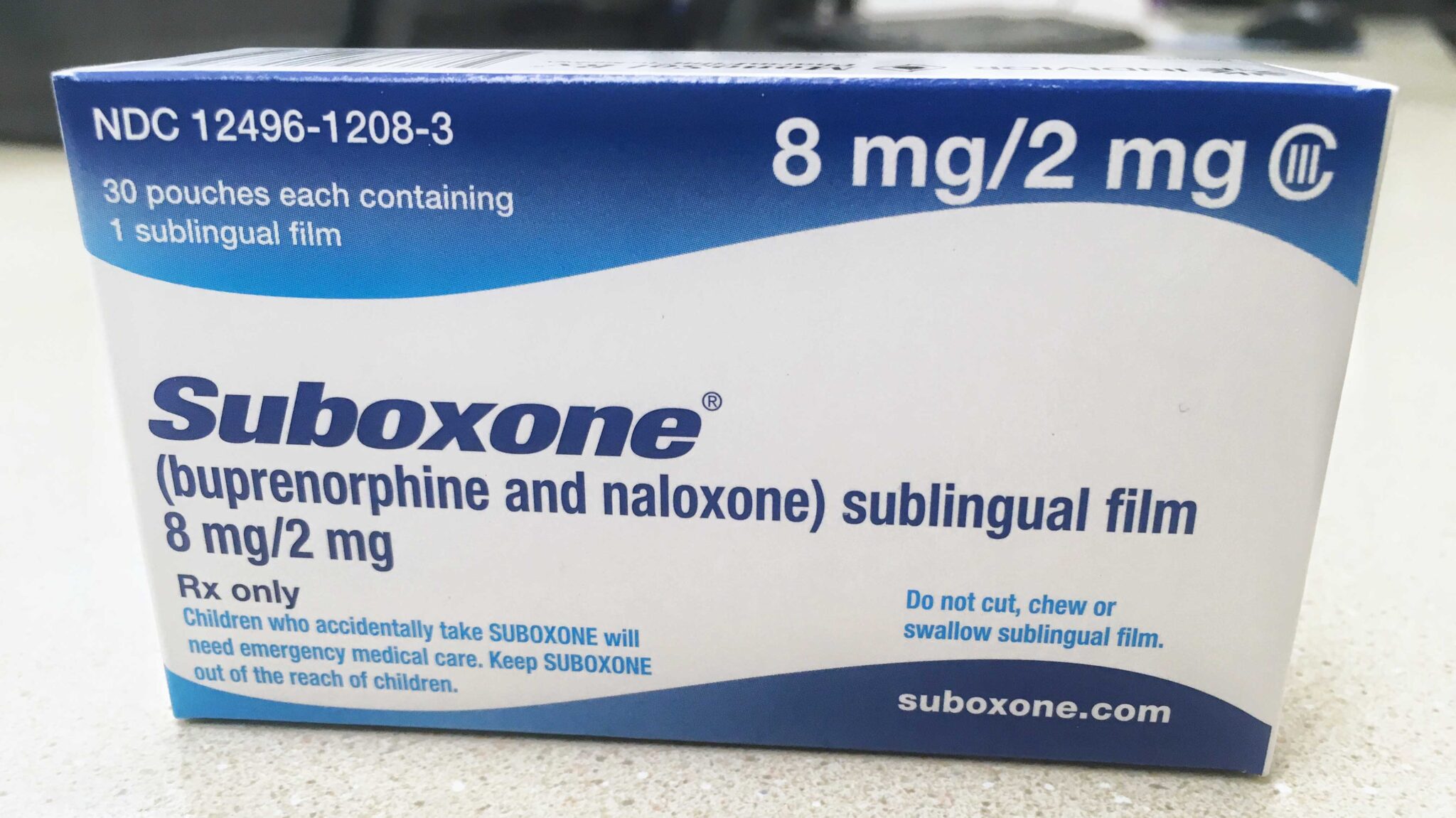
Suboxone, (buprenorphine and naloxone) is a Schedule III Controlled Substance. As laid out by the FDA, it is recommended to read through the medical guide and become familiar with possible adverse reactions, drug interactions, and the risk for abusing Suboxone. Suboxone is used to treat the notoriously uncomfortable withdrawal symptoms of opioid addiction. It’s composed of two drugs; buprenorphine and naloxone. Buprenorphine is a partial opioid agonist, while naloxone is a pure opioid antagonist. An opioid agonist excites opioid brain receptors. Pure opioid antagonists block opioids from reaching opioid brain receptors. When prescribed, Suboxone is available in two forms; soluble sublingual films and soluble sublingual tablets. Suboxone can also be prescribed to patients with no addiction or dependency history as a pain-management aide. Since it’s technically classified as an opiate, Suboxone could be an option for those suffering with pain that’s not associated, in any way, with addiction or chemical dependency.
How long does Suboxone block opiates?
Suboxone blocks opioid brain receptors and prevents withdrawal symptoms. Its full effects last anywhere from 24 – 60 hours. The best way to remember how long Suboxone blocks opiates is to think of the two drugs independently. Buprenorphine acts as an opiate blocker and naloxone functions to hinder the potential for abuse. When taken as prescribed, Suboxone begins blocking opiates within 40 – 120 minutes. It only takes minutes to fully dissolve under the tongue. If a patient is prescribed to take more than one film or tablet, they should place one on each side of the tongue. Suboxone films or tablets should only make contact with either side of the tongue, making sure to avoid the medications touching. If a patient ingests an opiate, (heroin, oxycodone, fentanyl, morphine), within 24 hours of taking Suboxone, it will not work or worse, the patient could enter a stage of withdrawal. Always be sure to read and follow the directions of your doctor, taking precautions to guard against misuse.
Having Success with Suboxone
There’s the argument, “If you take Suboxone, you’re not really clean and sober.” While it can be said that those who take Suboxone are substituting one for another, it’s not so simple. The whole of a person’s situation must be examined. Suboxone helps end the especially non-glamourous parts of addiction such as stealing to support the habit, “borrowing” from friends/family, or not eating or sleeping for days on end. If that’s the case, wouldn’t Suboxone be considered a success in that regard? Then comes that saying once again, “the lesser of two evils.” And perhaps so! After all, Suboxone is technically an opioid. The decision should include your family and those you consider close. Those familiar with Alcoholics Anonymous, know the Big Book. There’s a specific chapter entitled The Doctor’s Opinion. In it, lies mention of the “phenomenon of craving.” Naloxone, being a pure (or full) opioid antagonist, is especially effective in combating cravings. While naloxone is a “craving killer” buprenorphine is a partial opioid agonist and possesses some risk of abuse. However, with a collaborative effort including your doctor, counselors, and a solid support system, Suboxone is proven to be an effective tool in combating the nail-digging grips of opioid addiction. Any controlled substance comes with a risk. It might appear on the surface that it’s counterintuitive to use an opioid to treat an opioid addiction, but we must remember to weigh the pros and cons of taking Suboxone. Before beginning a Suboxone regimen, schedule a day to have a chat with your doctor. If you don’t know your doctor well enough to feel comfortable just yet, speak with someone who has had experience with Suboxone. It doesn’t necessarily have to be a medical professional but make sure you trust the person and hold them in high regard.
A Necessary Policy Change
Suboxone is clearly effective and addicts today who are seeking help, no longer need to jump through any cumbersome hoops to obtain a prescription. There is a significant reason for this change in policy. According to the Centers for Disease Control and Prevention, (CDC), there were over 90,000 overdose deaths to be estimated in a 12-month period as of September 2020. “Increases in overdose deaths emphasize the need to expand access to evidence-based treatments, including buprenorphine that can be prescribed in office-based settings,” said Assistant Secretary for Health, Rachel Levine, MD. “These guidelines provide another tool to help communities respond to the evolving overdose crisis, equipping providers to save lives in their communities.” Prior to this change, medical providers had to obtain a special number referred to as an “X” number. To receive an X number, a physician or medical provider would have had to take an 8-hour waiver course.
Medically-Assisted Treatment
Sustaining recovery and being a “normal” functioning member of society is the addict’s desired end game. Starting at an in-patient treatment facility is a good option. To learn your options for treatment, call the Rehab Helpline for Drugs and Alcohol at 877-467-4825. If inpatient treatment is not an option, there are plenty of out-patient treatment programs with high success rates. Finding treatment near you is easier than ever. MAT or medically-assisted treatment is an effective way to not only find peace within recovery but also helps deter the likelihood of an overdose. The purpose of MAT is long-term, sustainable recovery. By being proactive in the recovery process, other areas of life become better and easier to deal with. Now, life throws us as many curveballs as Zack Greinke in a 7-inning span. Overcoming our demons and staring down our cravings is no easy feat. Suboxone, paired with a proper treatment plan is only one of the ways to help you cope with your, (God-willing), newfound sobriety! Suboxone is not the only medication available for opioid addiction. There are similar-acting drugs such as Subutex (buprenorphine only), Methadone, and extended-release naltrexone, more commonly known by the brand name Vivitrol.

Tom Falcone is freelance copywriter and web developer, contributing regularly to various health, wellness, and financial publications.